WILLCOX, Arizona, August 17, 2015—Ask Sam Lindsey about
the importance of Northern Cochise Community Hospital and he’ll give you a wry
grin. You might as well be asking the 77-year-old city councilman to choose
between playing pickup basketball—as he still does most Fridays—and being
planted six feet under the Arizona dust.
Lindsey believes he’s above ground, and
still playing point guard down at the Mormon church, because of Northern
Cochise. Last Christmas, he suffered a severe stroke in his home. He survived,
he said, because his wife, Zenita, got him to the hospital within minutes. If
it hadn’t been there, she would have had to drive him 85 miles to Tucson Medical
Center.
There are approximately 2,300 rural
hospitals in the U.S., most of them concentrated in the Midwest and the South.
For a variety of reasons, many of them are struggling to survive.
In the last
five years, Congress has sharply reduced spending on Medicare, the federal
health insurance program for the elderly, and the patients at rural hospitals
tend to be older than those at urban or suburban ones. Rural hospitals in
sparsely populated areas see fewer patients but still have to maintain
emergency rooms and beds for acute care. They serve many people who are
uninsured and can’t afford to pay for the services they receive.
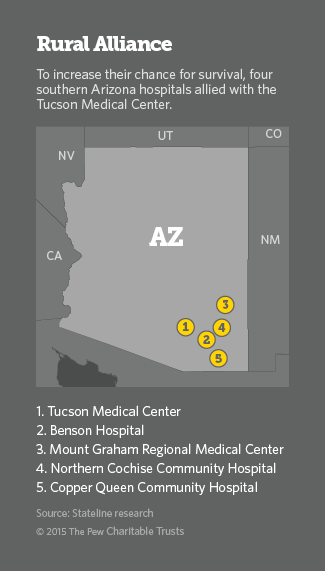
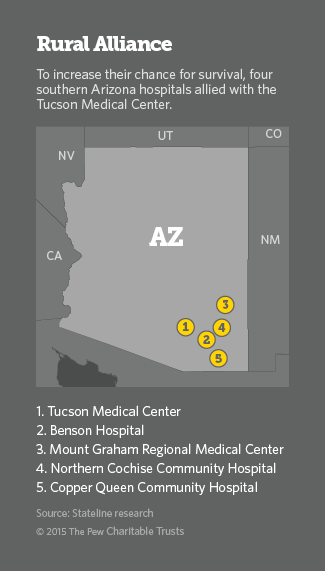 Several months ago, Northern Cochise
sought to strengthen its chances for survival by joining an alliance with
Tucson Medical Center and three other rural hospitals in southwestern Arizona.
Together, the Southern Arizona Hospital Alliance is negotiating better prices
on supplies and services. And the Tucson hospital has promised to help its
rural partners with medical training, information technology and doctor
recruitment.
Several months ago, Northern Cochise
sought to strengthen its chances for survival by joining an alliance with
Tucson Medical Center and three other rural hospitals in southwestern Arizona.
Together, the Southern Arizona Hospital Alliance is negotiating better prices
on supplies and services. And the Tucson hospital has promised to help its
rural partners with medical training, information technology and doctor
recruitment.
“We are committed to remaining
autonomous for as long as we can,” said Jared Wilhelm, director of community
relations at Northern Cochise. “We think this gives us the best leverage to do
so.”
Northern Cochise and the other rural
hospitals in the alliance, which is similar to ones in Kansas, Mississippi,
Washington state and Wisconsin, hope that by joining they will avoid the fate of 56 rural hospitals
that have closed since 2010. Another 283 rural hospitals are in danger of
closing, according to the National Rural Health Association (NRHA).
Right now, some Arizonans in the region
are learning what it’s like to lose a hospital. Cochise Regional Hospital, in
Douglas, near the Mexican border, closed earlier this month, following
Medicare’s decision to terminate payments because of repeated violations of
federal health and safety rules.
The hospital was part of a Chicago-based chain
and its closing leaves Arizona residents in the far southeastern portion of the
state up to 75 miles away from the closest hospital emergency room.
Sam Lindsey shudders to think what a
long drive to Tucson would have meant for him last Christmas.
“If I’d have had to go 85 miles,” he
said, “I don’t think I’d be here today.”
Multiple
Advantages
The alliance offers the rural members
multiple advantages. One of the most important is in purchasing. Their combined
size will enable them to get discounts that are beyond them now.
For example,
instead of being a lone, 49-bed hospital with limited bargaining leverage,
alliance member Mount Graham Regional Medical Center, in Safford, is suddenly
part of a purchasing entity with more than 700 beds.
“If I’m just Mount Graham and I’m going
to buy one MRI every seven years, the sales people will say, ‘Oh, that’s very
nice,’ ” said Keith Bryce, Mount Graham’s chief financial officer. “But as part
of this alliance that they want to do regular business with, they are going to
give us a much better price.”
Bryce said that he expects the added
purchasing power alone will save Mount Graham “in the six figures” every year.
Similarly, the hospitals expect the
combined size of the alliance to result in lower costs for employee benefits,
workers’ compensation and medical malpractice insurance.
The alliance also helps the rural
hospitals recruit doctors and other medical providers, many of whom are
reluctant to work, let alone live, in isolated areas.
Rural hospitals rarely
have the contacts and relationships that help urban hospitals find doctors.
“We’ve been trying to recruit another primary care doctor to this community for
the last year with no success,” said Rich Polheber, CEO of Benson Hospital,
another alliance member.
Tucson Medical Center has pledged to
use its own recruiting muscle to help its rural partners find providers who are
willing to live in rural areas, or at least regularly see patients there. As an
incentive, Tucson will offer interested doctors help in managing the business
aspects of their practices.
The rural alliance members also want
Tucson’s help with medical training and IT. Some have dipped into telemedicine,
which is particularly valuable for rural hospitals underserved by specialists,
and are looking to expand those efforts.
Copper Queen Community Hospital, in
Bisbee, the fourth rural member of the alliance and probably the rural hospital
in the best financial shape, is the most advanced user of telemedicine. Its
networks in cardiology, neurology, pulmonology and radiology can connect
doctors and their patients to specialists at major institutions such as the
Mayo Clinic and St. Luke’s Medical Center, in Phoenix.
The alliance also will make it easier
for patients who have surgery in Tucson to be transferred back to their home
hospitals for recovery and rehabilitation, saving them and their families from
traveling long distances.
A Defensive
Strategy
Despite the numerous advantages for the
rural partners, the idea for the alliance began with the Tucson hospital, which
approached the others with the proposal last spring. At the outset, some of the
rural hospitals were skeptical.
“At first, we were like, ‘OK, so why
are they doing this? What’s in it for them? Do they want to absorb us?’ ” said
Bryce, the Mount Graham CFO.
But after a series of meetings, the
suspicions disappeared and the rural hospitals eagerly signed on.
The Tucson hospital was frank about its
motivation: to remain independent in an industry moving toward consolidation.
As a result of acquisitions in the last few years, it is the last locally
owned, independent hospital in Tucson.
“All of a sudden, we were in a
situation where [Tucson Medical Center] found itself isolated and facing its
own competitive market pressures because the environment had so dramatically
changed,” said Susan Willis, executive director of market development at the
hospital and president of the new alliance.
Nearly a quarter of Tucson’s patients
come from outside the city, many from the areas served by the rural hospitals
in the new alliance. Cementing the relationship with those hospitals, Willis
said, will help Tucson maintain a flow of patients who need medical services
that are beyond the capabilities of the rural hospitals.
The rural members have
laboratories, diagnostic equipment and therapeutic services, but some have
little or no surgical or obstetrical services. Not one is equipped to perform
complicated surgeries.
“Certainly you could describe it as a
defensive strategy,” Willis said.
Decades of
Pressure
Many of the problems plaguing
rural hospitals date to 1983, when Medicare began paying hospitals a set fee
for medical services and procedures rather than reimbursing them for the actual
costs of providing that care.
From 1983 to 1998, 440 rural hospitals closed in
the U.S., according to the NRHA. That prompted Medicare to begin reimbursing
certain rural hospitals for their actual costs, which helped stabilize them.
But the recession hit rural hospitals
especially hard, as did 2011 budget cuts that reduced Medicare payments by 2
percent.
Because the rural population tends to be older, rural hospitals rely
heavily on Medicare payments. The pressure increased in 2012, when the federal
government reduced by 30 to 35 percent its reimbursements to hospitals for
Medicare patients who don’t cover their share of the bill.
“That’s an example of how a little
policy change that seems insignificant in Washington can have profound effects
in the rural areas,” said Brock Slabach, NHRA’s senior vice president for
member services.
Finally, more insurance plans are
increasing copayments and other out-of-pocket costs. Many of the patients at
rural hospitals have low incomes. And when they can’t cover their costs, the
hospitals have to pick up the tab.
“We don’t have cash reserves,” said
Polheber, the Benson Hospital CEO. “We live on the edge, day to day, week to
week. [The alliance] seemed like the best way to keep us going.”
Given the threats to the nation’s rural
hospitals, many are eager to learn from any models that work, which is why the
Arizona alliance has attracted notice.
Slabach, for one, calls it a promising
model, although one that may not be replicable everywhere.
“You have to have
willing partners willing to collaborate and provide assistance to each other,”
he said. “You need partners that share a cultural fit with you.”
The rural members of the alliance are
major employers in their communities and assets in attracting other employers
and residents, including the snowbirds, who flock to the area every winter.
But
hospital leaders, workers and patients say saving lives is the main reason the
hospitals must remain open.
“In medicine, distance lessens the
chances of survival,” said Pam Noland, director of nursing at Northern Cochise.
“Even if a patient has to be transferred to [Tucson Medical Center] or
somewhere else, stabilizing them here is the difference between life and
death.”